QPR Gatekeeper Training in Northwestern Pennsylvania

The Northwest Pennsylvania (NW PA) Veteran Suicide Prevention Program operates on a three-pronged approach involving healthcare providers, community organizations, and Veterans and their families in the 15 counties of NW PA.
This article summarizes the mission of the NW PA Veteran Suicide Prevention Program and provides an update on our QPR gatekeeper training efforts and the outcomes experienced thus far.
Read time: 7 minutes
An Update of Our Work and Outcomes
In 2020, the University of Pittsburgh School of Pharmacy’s Program Evaluation and Research Unit (PERU) and Janice Pringle, Ph.D., received $3,500,000 in funding from the U.S. Centers for Disease Control and Prevention’s (CDC) new Comprehensive Suicide Prevention Program for Veteran suicide prevention in Northwest Pennsylvania. PERU’s Northwest Pennsylvania Veteran Suicide Prevention Program (NW PA VSPP) is a collaborative effort between healthcare partners, community organizations, and Veterans groups to create significant and lasting change in the 15-county region. The program aims to reduce Veteran suicide attempts, injuries, and deaths by 10 percent (on average) over five years using the principles of the Zero Suicide framework and the Zero Suicide in Health and Behavioral Health Care model. Primary goals are improving access to treatment and support services, increasing awareness of suicide risk, and targeted suicide prevention activities and training opportunities.
Grounded in the Zero Suicide Model
 Suicide is a growing public health crisis that took more than 48,000 lives in the United States in 2021, according to the CDC. In Pennsylvania alone, the rate of suicide deaths in 2020 was 13.25 per 100,000, compared to the national rate of 13.96 per 100,000.[1]
Suicide is a growing public health crisis that took more than 48,000 lives in the United States in 2021, according to the CDC. In Pennsylvania alone, the rate of suicide deaths in 2020 was 13.25 per 100,000, compared to the national rate of 13.96 per 100,000.[1]
The Zero Suicide framework is based on the realization that people experiencing suicidal thoughts and urges often do not receive the care they need from a sometimes fragmented and distracted health care system. Studies have shown that most people who died by suicide saw a health care provider in the year before their deaths.[2] This information presents an opportunity for healthcare systems to make a real difference by transforming patient screening processes and the care they receive. Throughout all 50 states and internationally, health and behavioral health systems implementing Zero Suicide have found success by adapting the model through the lenses of their care offerings and cultural considerations.
The Role of the Gatekeeper in Reducing Veteran Suicide
 Suicide is an important problem affecting military service members and Veterans. Recent estimates suggest that 17 Veterans may die by suicide each day.[3] To address this serious problem, the U.S. Department of Defense and the U.S. Department of Veterans Affairs have implemented comprehensive suicide prevention programs that reduce the negative attitudes and stigma associated with mental health care.
Suicide is an important problem affecting military service members and Veterans. Recent estimates suggest that 17 Veterans may die by suicide each day.[3] To address this serious problem, the U.S. Department of Defense and the U.S. Department of Veterans Affairs have implemented comprehensive suicide prevention programs that reduce the negative attitudes and stigma associated with mental health care.
Stigma poses a significant barrier to seeking help, engaging in care, and completing psychological health treatment. Mental health stigma in the military is strongly grounded in military culture and is linked to a desire to handle problems independently. As a result, Veterans often refrain from seeking mental health services due to the stigma attached, which can lead to extreme and life-threatening consequences, including depression, substance use disorder, and suicide.
In 2004, the Garrett Lee Smith Memorial Act prioritized training suicide prevention gatekeepers. These training programs are designed to improve knowledge, skills, and motivation to prevent suicide. A gatekeeper is an individual who can recognize a crisis and the warning signs of someone possibly contemplating suicide. Gatekeepers come from all walks of life and do not require any prior training or education.
Clinical providers and nonclinical individuals interacting with Veterans and their families are natural gatekeepers to identifying and referring Veterans at risk for suicide. Gatekeeper training programs have improved knowledge and self-efficacy, especially among non-clinicians[4], and can help reduce the stigma associated with mental health care for at-risk Veterans.
QPR Gatekeeper Training in Northwestern Pennsylvania
 In 2022, the NW PA VSPP began delivering in-person and virtual QPR gatekeeper training at no cost to those living or working in the 15-county region. QPR, which stands for Question, Persuade, and Refer, equips people to recognize the warning signs of a suicide crisis and how to question, persuade, and refer someone to help. QPR is considered an emergency mental health intervention with the intent of identifying and interrupting the crisis and directing that person to proper care.
In 2022, the NW PA VSPP began delivering in-person and virtual QPR gatekeeper training at no cost to those living or working in the 15-county region. QPR, which stands for Question, Persuade, and Refer, equips people to recognize the warning signs of a suicide crisis and how to question, persuade, and refer someone to help. QPR is considered an emergency mental health intervention with the intent of identifying and interrupting the crisis and directing that person to proper care.
Components of the NW PA VSPP’s QPR Gatekeeper Training
- How to Question, Persuade, and Refer someone who may be suicidal
- The common causes of suicidal behavior and warning signs of suicide
- How to get help for someone in crisis
- Resiliency and protective factors within the Veterans community
QPR Training Outcomes to Date
 While CDC funding for training and outreach continues through August 2025, data collection and evaluation efforts are ongoing. Between March 2022 and February 2023, the NW PA VSPP conducted 38 in-person and virtual gatekeeper sessions resulting in 793 individuals learning about the QPR method. Of these participants, 298 self-identified as professionals trained in physical or behavioral healthcare, and 495 as working outside healthcare.
While CDC funding for training and outreach continues through August 2025, data collection and evaluation efforts are ongoing. Between March 2022 and February 2023, the NW PA VSPP conducted 38 in-person and virtual gatekeeper sessions resulting in 793 individuals learning about the QPR method. Of these participants, 298 self-identified as professionals trained in physical or behavioral healthcare, and 495 as working outside healthcare.
All QPR training sessions include a knowledge-based pre- and post-test designed to capture each participant’s level of understanding about the risks and signs of suicide and their confidence level activating the QPR steps. Evaluation data from individuals who participated in training between May 2022 and October 2022 indicates that 76% of participants scored 80% or higher on the training post-test.
Applying Information from the Training
Participants felt more confident and comfortable asking questions about suicidal ideation and having follow-up conversations with their clients. According to them, this confidence and comfort would help them engage and interact. Other respondents mentioned they would apply the information to look for and identify signs of suicidal thoughts and ideation. Respondents mentioned the training information will help them to step in and handle a situation if it arises.
Changes in Self-Perception of Skills
Participants were asked to rate their perception of their knowledge and abilities concerning suicide awareness and assisting someone contemplating suicide. Figures 1, 2, and 3 show the response rates.
Figure 1 shows the responses for targeted suicide awareness knowledge and abilities. Before training, some participants did not feel confident in their knowledge and skills. After training, no participants indicated low confidence about suicide prevention. Specifically, after training, participants felt highly capable of recognizing warning signs.
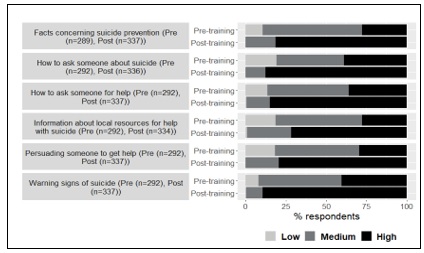
Figure 1. Change in ratings for targeted suicide awareness abilities.
Figure 2 shows participants’ understanding of suicide and suicide prevention. Before training, some participants reported a low understanding. After training, there was a substantial improvement.
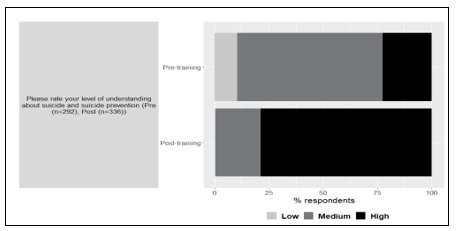
Figure 2. Change in participant understanding of suicide and suicide prevention.
Figure 3 displays participants’ responses to how likely they are to ask someone about suicide and if it is appropriate to ask. Some disagreement existed prior to, but, more importantly, some disagreement continued to persist even after training. This finding presents an area for improvement to better understand the hesitancy of some participants to engage in questioning.
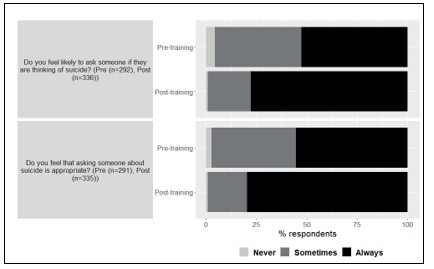
Figure 3. Change in rating for asking about suicide and appropriateness.
Looking Ahead
Participating in QPR gatekeeper training can be an effective way to learn more about the causes of suicide and develop suicide prevention skills. For Veterans and those in their community/family network, recognizing the warning signs of suicide are vital. Developing the comfort and confidence using QPR with a friend, family member, client, or community member can help those in crisis access behavioral healthcare and needed services. To learn more about the NW PA VSPP and participate in our training and outreach, visit resilientveteran.org.
Sources
[1] Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS) [Online]. (2023)
[2] Raue PJ, Ghesquiere AR, Bruce ML. Suicide risk in primary care: identification and management in older adults. Curr Psychiatry Rep. 2014 Sep;16(9):466. doi: 10.1007/s11920-014-0466-8. PMID: 25030971; PMCID: PMC4137406.
[3] Department of Veteran’s Affairs: 2021 National Veteran Suicide Prevention Annual Report. 2021. [Accessed: Sep 9, 2021]. Available from URL: https://www.mentalhealth.va.gov/docs/data-sheets/2021/2021-National-Veteran- Suicide-Prevention-Annual-Report-FINAL-9-8-21.pdf
[4] Matthieu MM, Cross W, Batres AR, Flora CM, Knox KL. Evaluation of gatekeeper training for suicide prevention in veterans. Arch Suicide Res. 2008;12(2):148-54. doi: 10.1080/13811110701857491. PMID: 18340597.
Share Our Vision and Get Involved
Our Vision: The work of the Northwest Pennsylvania Veteran Suicide Prevention Program will result in resident Veteran suicides being reduced to zero by the end of the project period (August 31, 2025).
Whether you identify as a healthcare provider, community organization, or Veteran, there are several opportunities through the NW PA Veteran Suicide Prevention Program and PERU to connect to resources, participate in educational training, and promote harm reduction strategies. We are actively recruiting healthcare and community partners to work with us in meeting our goals and objectives. To learn more, visit the program website at theresilientveteran.org.
Need Help? Know Someone Who Does? Contact the National Suicide Prevention Lifeline at 988 or use the online Lifeline Crisis Chat. Both are free and confidential. You’ll be connected to a skilled, trained counselor in your area.

